INSIGHTS is a one-stop location for the latest trends, industry and company news from Bala's engineering experts.
AIA Accredited Courses from Bala
Bala's experts have developed a wide range of AIA Accredited courses for our clients and partners to increase industry knowledge and understand the latest technologies and trends.
Click HERE for a full list of seminars. To set up a lunch or request additional information please email info@bala.com.

MEP/FP
- Infrastructure Considerations for Converting Commercial Office Building to Multifamily Residential
- A2L Refrigerants & Code Implications
- Energy Modeling Strategies
- Energy Code Changes and How They Effect Your Projects
- Chilled Beam Technology - Architectural & Energy Advantages
- Converting Office Space for Lab Ready Use
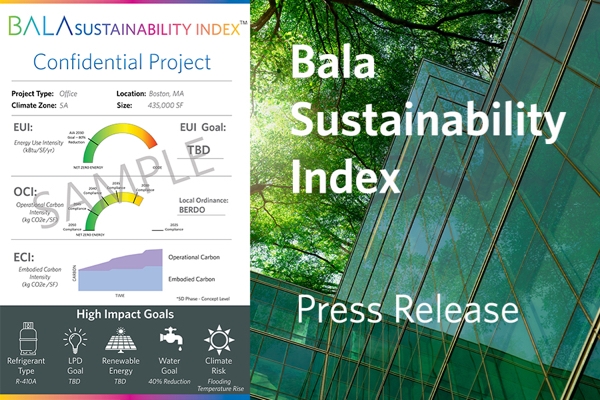
Sustainability
- Climate Risk & Resiliency (HSW Credit)
- Building Electrification
- Net Zero Labs
- WELL vs Fitwel
- Whole Building Life Cycle Analysis
Technology
- Building Systems Integration
- Designing for Responsive Building, Smart Buildings, IoT and User Experience
- Healthcare Technology Trends
- Technology Integration into Conferencing Collaboration Spaces
- Technology Choices for Multi-Family Projects
Structures
- Structural Considerations for an Existing Building
- Warehousing Structural Systems
- Mass Timber